Exclusion for dentists?
Adella Bedella
19 years ago
Related Stories

WORKING WITH PROS10 Things Decorators Want You to Know About What They Do
They do more than pick pretty colors. Here's what decorators can do for you — and how you can help them
Full Story
COMMUNITYTour a Pioneering Beach Town That Fosters Community
No cars, mixed-use zones, strict building codes ... a new book takes us inside Seaside, a champion of New Urbanism
Full Story
ARCHITECTURE8 Modern Hamptons Homes Buck Convention
Defying the overblown architecture popular in this affluent Long Island area, these modern residences take a more modest approach
Full Story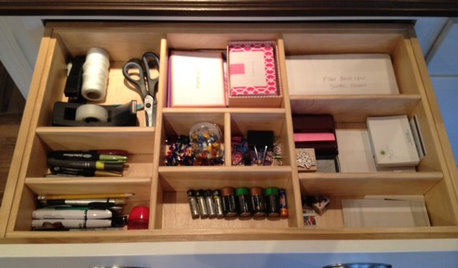
HOUSEKEEPINGGet It Done: Whip That Junk Drawer Into Shape
If the jumbled mess in your catch-all drawer inspires only dread, this quick organizing project is just the sort you need
Full Story
HouzzLenz: The New Way to See Your Home
This amazing new technology promises to revolutionize home design. Here’s how it works
Full Story
INSIDE HOUZZHouzz Survey: See the Latest Benchmarks on Remodeling Costs and More
The annual Houzz & Home survey reveals what you can expect to pay for a renovation project and how long it may take
Full Story
LIFEHow to Decide on a New Town
These considerations will help you evaluate a region and a neighborhood, so you can make the right move
Full Story
REMODELING GUIDESContractor Fees, Demystified
Learn what a contractor’s markups cover — and why they’re worth it
Full StorySponsored
More Discussions



dstanek
Adella BedellaOriginal Author
Related Discussions
PCHP major gripe!
Q
Anyone else have sensitive teeth?
Q
Freeway Noise Suggestion
Q
Does your dental hygienist take your blood pressure before a cleaning?
Q
trekaren
beache
Sully6
Nancy in Mich
kathyg_in_mi